Recently Platelet Rich Plasma (PRP), which comes from your own blood, has surfaced strongly in plastic surgery, used for a variety of issues including wound healing, diabetic ulcers, dermatology and aesthetic applications.
PRP has been proven to promote wound healing. It also has a positive effect when used with face-lifts as it increases skin volume, aids skin rejuvenation & regeneration and improves wrinkling.
The clinical application of PRP is based on an increased number of growth factors (GFs) that are released by these concentrated platelets, and from the secretion of proteins which trigger and accelerate the healing process at a cellular level.
This treatment helps to restore natural beauty by starting the rejuvenation process of the skin, aiming to keep and maintain it in a more youthful state. This happens because the skin is encouraged to function more like a younger version of itself, thanks to the procedure.
So, youth IS in your blood - the magical powers are contained in the platelet factors.
The History
Platelet-rich plasma (PRP), also known as platelet-rich growth factors (GFs), started in the field of haematology1. Haematologists created the term PRP in the 1970s to describe plasma which has a platelet count above that of peripheral blood. This was initially used as a transfusion product to treat patients with a low platelet count, which caused them to have a bleeding tendency 2.
Ten years later PRP debuted in maxillofacial surgery - used for its blood clotting, anti-inflammatory and wound-healing effects3. Other medical fields that use PRP include heart surgery, paediatric surgery and plastic surgery (where it is used in skin rejuvenation, for the treatment of hair loss and for scar revision4, 5,6-14).
Wounds have a pro-inflammatory biochemical environment (i.e. a lot of inflammation is present) that impairs healing in chronic wounds. In cosmetic dermatology, a study performed in a laboratory demonstrated that PRP could stimulate human skin fibroblast proliferation and increase collagen synthesis13. Additionally, based on histological evidence, PRP injected into human skin induces soft-tissue growth and new collagen formation, as well as stimulating new blood vessel and fat tissue formation14, 15. The result is a thicker healthier skin.
A further application of PRP is the improvement of scars resulting from burns, surgery and acne 16. In 2006 PRP started to be considered a potential treatment for promoting hair growth and has been suggested as a new therapy for hair loss17, 18. The benefits include:
- stimulation of hair growth;
- prevention of hair fall;
- improvement of the hair shaft, stem and calibre (thickness);
- an increase in shine, vitality and pliability; and
- a reduction in hair-splitting and breakage.
The function of the blood platelet
Platelets develop from the bone marrow. Their main function is to contribute to blood clotting. They are activated when an injury occurs19 to stop the bleeding.
Platelets were initially thought to have only blood clotting activity. In recent years scientific research has provided a new perspective on platelets and their functions. Studies suggest that platelets contain an abundance of growth factors (GFs) and chemical substances that can affect inflammation, new blood vessel growth, stem cell migration and cell proliferation20, and 21,22.
Where does PRP come from?
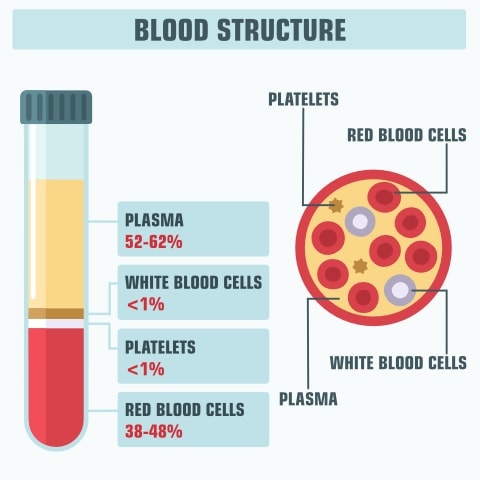
The PRP is obtained from the blood of the patient (typically around 20 ml of blood is collected from a vein in the forearm), which is then placed in a centrifuge. After centrifugation the separation of blood components (red blood cells, PRP, and platelet-poor plasma) follows – this is due to the different density of each component. The separated platelets and plasma are then prepared for injection into the skin, and the area immediately below the skin, of the zone that is to be treated.
When centrifuged, blood separates into different components depending on the density of the red blood cells, white blood cells, platelets and plasma.
The growth factors (GFs) in PRP promote 4 main actions at the injection site, namely:
- the proliferation of cells,
- the migration of stem cells to the area of injection,
- cell differentiation of the stem cells into different tissue-producing types, and
- new blood vessel growth 22,25-32.
How is it used in a facial?
The Platelet Rich Plasma is used on the face to address areas of concern. The balance of the Platelet Poor Plasma (PPP) can be injected into the hands, neck or chest for mild, general rejuvenation.
The PRP is applied to the areas of the face in 2 ways, depending on the requirements of the patient and the recommendation of the doctor:
- injected directly into the areas of concern using the mesotherapy technique, or
- applied over the skin after microneedling (using a Dermapen for example).
Please remember that the more aggressive the needling the more inflamed and red your skin will be at the end of the treatment, so definitely combine with our GF1 Aftercare product to shorten your recovery time and prevent pain and infection.
Long-term effects and popularity of the PRP procedure
Kim K made headlines when she tried the treatment in 2013, but she's not the only star who has indulged in the PRP or “Vampire (Dracula) Facial” as it is sometimes referred to.
Her older sister and fellow reality TV icon, Kourtney, extolled the benefits of PRP on her premium app last November, saying it was 'SO beneficial'.
Others, including British actor Rupert Everett, and Israeli model Bar Refaeli, are devoted fans of the gruesome procedure it has been claimed.
But “despite its popularity, existing evidence to support the clinical efficacy of PRP is limited” researchers wrote in a new review33.
Fourteen of the studies evaluated the use of PRP for facial rejuvenation. All the trials had positive outcomes and the treatment helped to decrease the appearance of wrinkles.
A further six studies reviewed delved into the effects of the procedure in treating androgenic alopecia, also known as pattern baldness.
Each reported a good result in terms of hair regrowth, according to the review in the Journal of Plastic and Reconstructive Surgery.
The final two studies showed PRP worked to treat facial acne scars, as reported by Dr Hazen and his colleagues in the official journal of the ASPS.
Further trials needed
But despite these encouraging results, the review highlighted several shortcomings in the evidence on PRP for facial aesthetic procedures.
Dr Hazen and co-authors warned that the methods of PRP preparation and injection varied considerably, with some studies giving no information on this part of the procedure.
The trials also lacked detailed assessments in terms of the skin quality before and after the PRP treatment. Few of the studies used control groups, which are desired in most trials of this nature.
Some of the experiments also failed to follow-up with their patients to find out if the benefits of the costly PRP injections had persisted for any length of time.
The role of Hypochlorous acid in assisting the PRP procedure
Like any other invasive procedure, the risk factors leading to possible complications like infection, bleeding, biofilm formation, excessive inflammation and swelling must be carefully controlled. Topically applied HOCl is emerging as an option with a broad range of potential uses. It is antimicrobial, anti-inflammatory and antipruritic. It increases oxygenation to healing wounds and is active against biofilm. HOCl is a pH 5.5 oxydation/reduction agent made to emulate nature. In our clinical experience, it has proven useful across an assortment of cosmetic and medical dermatologic procedures and would be beneficial for a range of additional medical dermatology presentations, such as pruritus post-operatively.
Thoclor GF1 Aftercare was specially formulated to assist the clinician in preparing the skin pre-operatively by sterilising it and initiating an anti-inflammatory response. Post-operatively it assists in preventing infection and with the healing process, whilst also controlling pain and inflammation34 .
Conclusion
Platelet-rich Plasma (PRP), when used in a facial, is a great way to increase skin volume, aid skin rejuvenation & regeneration and improve wrinkling. Using your own blood, which is spun, separated and then injected back into the skin, this is an effective natural alternative to fillers with longer-lasting results.
As always we recommend using a qualified therapist or aesthetic doctor for procedures like these, ensuring they have the proper equipment and treatment facilities. Combine with our GF1 Aftercare product to reduce pain & inflammation as well as to minimise your risk of post-treatment infection.
Please do note that the results are temporary, peaking after about 3 months and then slowly tapering off over a period of anywhere from 9 months up to 2 years. To maintain the effects you will need to repeat the procedure. If you are doing a series of these treatments then make sure to wait at least a month between each, giving your skin a chance to recover.
References
- Andia I, Abate M: Platelet rich plasma: underlying biology and clinical correlates. Regen Med 2013; 8: 645–658.
- Andia I: Platelet-rich plasma biology; in Alves R, Grimalt R (eds): Clinical Indications and Treatment Protocols with Platelet-Rich Plasma in Dermatology. Barcelona, Ediciones Mayo, 2016, pp 3–15.
- Conde Montero E, Fernandez Santos ME, Suarez Fernandez R: Platelet-rich plasma: applications in dermatology. Actas Dermosifiliogr 2015; 106: 104–111.
- Lynch MD, Bashir S: Applications of platelet rich plasma in dermatology: a critical appraisal of the literature. J Dermatolog Treat 2016; 27: 285–289.
- Andia E, Rubio-Azpeitia J, Martin I, Abate M: Current concepts and translational uses of platelet rich plasma biotechnology; in Ekin - ci D (ed.): Biotechnology. InTech, 2015, DOI: 10.5772/59954. https://www.intechopen.com/books/biotechnology/current-concepts-and-translational-uses-of-plateletrich-plasma-biotechnology.
- Li ZJ, Choi HI, Choi DK, Sohn KC, Im M, Seo YJ, Lee YH, et al: Autologous platelet-rich plasma: a potential therapeutic tool for promoting hair growth. Dermatol Surg 2012; 38: 1040–1046.
- Sommeling CE, Heyneman A, Hoeksema H, Verbelen J, Stillaert FB, Monstrey S: The use of platelet-rich plasma in plastic surgery: a systematic review. J Plast Reconstr Aesthet Surg 2013; 66: 301–311.
- Salazar-Alvarez AE, Riera-del-Moral LF, Garcia-Arranz M, Alvarez-Garcia J, Concepcion- Rodriguez NA, Riera-de-Cubas L: Use of platelet-rich plasma in the healing of chronic ulcers of the lower extremity. Actas Dermosifiliogr 2014; 105: 597–604.
- Picard F, Hersant B, Bosc R, Meningaud JP: Should we use platelet-rich plasma as an adjunct therapy to treat “acute wounds”, “burns”, and “laser therapies”: a review and a proposal of a quality criteria checklist for further studies. Wound Repair Regen 2015; 23: 163–170.
- Cobos R, Aizpuru F, Parraza N, Anitua E, Orive G: Effectiveness and efficiency of platelet rich plasma in the treatment of diabetic ulcers. Curr Pharm Biotechnol 2015; 16: 630–634.
- Sclafani AP, Azzi J: Platelet preparations for use in facial rejuvenation and wound healing: a critical review of current literature. Aesthec Plast Surg 2015; 39: 495–505.
- Conde Montero E: PRP in wound healing; in Alves R, Grimalt R (eds): Clinical Indications and Treatment Protocols with Platelet-Rich Plasma in Dermatology. Barcelona, Ediciones Mayo, 2016, pp 59–72.
- Kim DH, Je YJ, Kim CD, Lee YH, Seo YJ, Lee JH, Lee Y: Can platelet-rich plasma be used for skin rejuvenation? Evaluation of effects of platelet-rich plasma on human dermal fibroblast. Ann Dermatol 2011; 23: 424–431.
- Sclafani AP, McCormick SA: Induction of dermal collagenesis, angiogenesis, and adipogenesis in human skin by injection of platelet- rich fibrin matrix. Arch Facial Plast Surg 2012; 14: 132–136.
- Lola Bou Camps: PRP in cosmetic dermatology; in Alves R, Grimalt R (eds): Clinical Indications and Treatment Protocols with Platelet-Rich Plasma in Dermatology. Barcelona, Ediciones Mayo, 2016, pp 45–57.
- o L: PRP and other applications in dermatology; in Alves R, Grimalt R (eds): Clinical Indications and Treatment Protocols with Platelet-Rich Plasma in Dermatology. Barcelona, Ediciones Mayo, 2016, pp 73–78.
- Giordano S, Romeo M, Lankinen P: Plateletrich plasma for androgenetic alopecia: does it work? Evidence from meta analysis. J CosmetDermatol 2017, Epub ahead of print.
- Ayatollahi A, Hosseini H, Gholami J, Mirminachi B, Firooz F, Firooz A: Platelet rich plasma for treatment of non-scarring hair loss: systematic review of literature. J Dermatolog Treat 2017, Epub ahead of print.
- Theml H: Physiology and pathophysiology of blood cells; in Theml H, Diem H, Haferlach T (eds): Color Atlas of Hematology. Stuttgart, Thieme, 2004.
- Harmon K, Hanson R, Bowen J, Greenberg S, Magaziner E, Vandenbosch J, et al: Guidelines for the use of platelet rich plasma. https://www.scribd.com/document/159334949/206-ICMS-Guidelines-for-the-Use-of-Platelet-Rich-Plasma-Draftob-oasbonasdandbowndoww
- Ferrando J, Fernandez-Sartorio C, Gonzalez de Coss.o AC, Navarra E: Tratamiento de la alopecia androgenetica con factores de crecimiento plaquetario. Monografias Dermatologica 2016; 42: 491–497.
- Alves R, Grimalt R: A randomized placebo controlled, double-blind, half-head study to assess the efficacy of platelet-rich plasma on the treatment of androgenetic alopecia. Dermatol Surg 2016; 42: 491–497.
- Wroblewski AP, Melia HJ, Wright VJ: Application of platelet-rich plasma to enhance tissue repair. Oper Tech Orthop 2010; 20: 98–105.
- Graziani F, Ivanovski S, Cei S, Ducci F, Tonetti M, Gabriele M: The in vitro effect of different PRP concentrations on osteoblasts and fibroblasts. Clin Oral Implants Res 2006; 17: 212–219.
- Gupta AK, Carviel J: A mechanistic model of platelet-rich plasma treatment for androgenetic alopecia. Dermatol Surg 2016; 42: 1335–1339.
- Uebel CO, da Silva JB, Cantarelli D, Martins P: The role of platelet plasma growth factors in male pattern baldness surgery. Plast Reconstr Surg 2006; 118: 1458–1466.
- Takikawa M, Nakamura S, Nakamura S, Ishirara M, Kishimoto S, Sasaki K: Enhanced effect of platelet-rich plasma containing a new carrier on hair growth. Dermatol Surg 2011; 37: 1721–1729.
- Paus R: Do we need hair follicle stem cells, hair follicle neogenesis to cure common hair loss disorders? Hair Transplant Forum Int 2008; 18: 89–90.
- Lin WH, Xiang LJ, Shi HX, Zhang J, Jiang LP, Cai PT, et al. Fibroblast growth factors stimulate hair growth through β-catenin and Shh expression in C57BL/6 mice. Biomed Res Int 2015; 2015: 73017.
- Jain R, De-Eknamkul W: Potential targets in the discovery of new hair growth promoters for androgenic alopecia. Expert Opin Ther Targets 2014; 18: 787–806.
- Akiyama M, Smith LT, Holbrook KA: Growth factor and growth factor receptor localization in the hair follicle bulge and associated tissue in human fetus. J Invest Dermatol 1996; 106: 391–396.
- Myung PS, Takeo M, Ito M, Atit RP: Epithelial Wnt ligand secretion is required for adult hair follicle growth and regeneration. J Invest Dermatol 2013; 133: 31–41.
- Hazen, A et al. Evaluating Platelet-Rich Therapy for Facial Aesthetics and Alopecia: A Critical Review of the Literature Plastic and Reconstructive Surgery: May 2018 - Volume 141 - Issue 5 - p 1115–1123
- Ashish Bhatia et al. Optimizing Wound Healing for Cosmetic and Medical Dermatologic Practical Dermatology March 2018, p 42-45