As we age we expect to see fluctuations in the way we look, from gaining a few extra inches around the waistline or seeing a few more wrinkles in the face looking back in the mirror. But did you know that the ageing you see on your skin is not entirely caused by time? About 20% of the changes in the appearance of the skin are down to genetics, the pre-determined rate at which you age. This is called intrinsic or chronological ageing. Unfortunately, a gigantic 80% of the alterations you see in your skin are caused by extrinsic factors – things like the sun, alcohol, pollution, diet, smoking and an assault from various chemicals in cosmetic products. These factors lead to premature ageing on the skin.
The structure of our skin
As you probably know the skin is the largest organ of the body, weighing approximately 4kg in the average adult. The thinnest skin occurs under the eyes and behind the ears, although men have thicker skin than women.
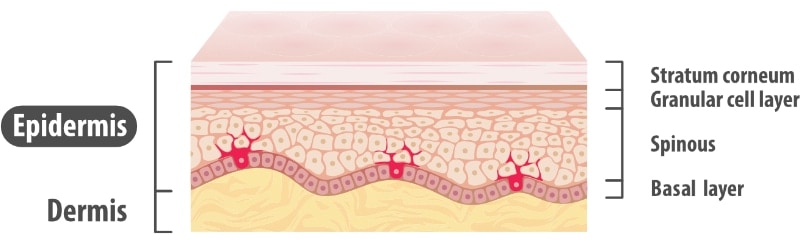
The skin is a compound organ consisting of 2 layers, namely the outer epidermis and inner dermis. Every square centimetre contains approximately 70cm of blood vessels, 55cm of nerves, 100 sweat glands, 15 oil glands and 230 sensory receptors. The half a million cells in this cm2 are constantly dying and being replaced. It’s a busy place.
The Epidermis
The thin outermost layer of the skin which is exposed to the environment, and is sensitive to the sun & free radical damage. The main types of skin cells in this outer layer of skin are:
- Keratinocytes: these are the basic cells of the skin.
- Melanocytes: these produce the skins natural pigmentation, or melanin. We all have a similar number of these cells but they don’t produce the same amount of melanin in each of us. The difference in the amount of melanin produced accounts for our different skin tones. These cells absorb UV light to protect the deeper layers of the skin from damage, and in doing so they change colour (depending on your skin type) leaving you with a tan – which is simply an overproduction of melanin. Melanocytes also occur in the hair follicles and are responsible for the colour of our hair.
- Langerhans cells: are responsible for your skin’s immunity. These cells repair damaged cells, or destroy those that are delinquent and could become cancerous. These cells themselves are very sensitive to UV – if they are damaged or destroyed your skin’s ability to repair itself is compromised.
- Stratum corneum: this is the horny outer part of the skin, made up of between 18 and 23 layers of flat, dry skin cells which are cemented together into a defensive wall. This layer is most important, again protecting from UV radiation and mechanical threat. This layer is easily damaged by the sun, trauma and chemicals.
The Dermis
This is the bottom layer of the skin and contains collagen and elastin, acting as a supportive mattress to the epidermis.
The dermis is made of about 95% collagen, which is important for the tone and structure of the skin. Elastin makes up a further 3% of the dermis, adding elasticity to the skin. Fibroblast cells are the main type of connective tissue cells and produce collagen and elastin.
Skin types and their reactions to sunlight
Whilst we all have a dermis and an epidermis we don’t all have the same skin type. The amount of melanin made by our melanocytes varies, leaving us with different skin tones and colours. These have been categorised in various ways, included here is the Fitzpatrick scale.
Type I
- hair: red or blond
- eyes: blue, grey or green
- skin: pale white, white with freckles
- burn easily in the sun, never tans
- highly susceptible to premature ageing and skin cancers from UV
Type II
- hair: blond, red, light brown
- eyes: blue, grey, green, hazel
- skin: pale white
- burn easily in the sun, tan lightly with repeated exposure
- high risk for skin cancer
Type III
- hair: chestnut or dark blond
- eyes: brown, blue, grey, green, hazel
- skin: olive, light brown
- sometimes burns, gradually tans
- skin cancer risk high with extreme exposure
Type IV
- hair: medium to dark brown
- eyes: brown, hazel
- skin: olive-looking, light to medium brown
- seldom burn, tan easily
- avoid extreme sun exposure to reduce skin cancer risk & pigmentation
Type V
- hair: dark brown
- eyes: brown
- skin: olive or dark brown
- tan easily & rarely burn.
- watch out for uneven skin tone & pigmentation from UV exposure
Type VI
- hair: very dark or black
- eyes: brown
- skin: very dark brown or black
- rarely burn
- watch out for uneven skin tone & pigmentation from UV exposure
Some of us tan, and some of us burn, depending on our skin types. But no matter the amount of melanin in our skins, sun exposure damages every skin in many ways. Firstly, it attacks the epidermis. The sun also damages the upper layers of the dermis. Once fibroblast cells in the dermis are damaged by UV penetration or free radical activity, they begin to make defective collagen and elastin. This leads to a change in tone, structure and elasticity. The dermis becomes thinner and less resilient, prone to wrinkling and sagging with a loss of tautness.
Sun protection
We now know that sun damage builds up over time and that we should use sun protection every day – even if it is cloudy and we are staying indoors. Radiation from our computers, smartphones and other devices also has an impact on our skins and contributes to its ageing. To protect your skin from the sun, and skin cancer, you need to choose a broad-spectrum sunscreen that shields you from:
- UVB – the burning ray
This short-wave, intense, ultraviolet light radiates from the sun. UVB rays only penetrate the top layer of the skin (the epidermis) causing it to show a visible burn, which is the first warning sign that your skin is being physically damaged, characterised by redness and blistering. Older sunscreens on the market protect only against UVB rays and so prevent sunburn but don’t reduce your risk of skin cancer. - UVA – the ageing ray
These long-wave, intense ultraviolet rays can deeply penetrate the skin. UVA goes straight through the top layer of the skin and into the dermis These rays cause sun damage to the skin in the form of dryness, wrinkling and discolouration. They also damage the fibroblast cells, affecting the production of collagen and elastin. Unlike the burn you get from UVB rays, the effects of UVA sun damage are not immediately apparent. Failure to block UVA is the reason that dark spots on the skin get worse. - UVC – the cancer ray
This is potentially the most dangerous UV radiation. It is predominantly screened out by the ozone layer and is not normally a problem. UVC rays fatally mutate DNA and these changes cannot be prevented by sunscreens.
Both UV-A and -B deplete the skin of Langerhans cells, which are responsible for the immunity of the skin. Ultra-violet light’s greatest danger is the development of skin cancer; this is due to the formation of free radicals by UV light as well as the impairment of the local immune system in the skin.
The UVB rays of sunlight are more intense than UVA rays, and older sunscreen absorbed only these rays. The problem arose when people started applying sunscreens to prevent sunburns and ended up staying out in the sun longer than they ever could before. The result: More UVA damage and an increased incidence of skin cancer.
An ideal sunscreen should absorb or scatter all the harmful UV-rays, be non-toxic, non-irritating and non-allergenic. It should leave a pleasant feeling on the skin after application. The ideal sunscreen should also be easily formulated and compatible with a variety of ingredients. It should not have any taste or aftertaste, not discolour the skin or clothes, nor produce unpleasant odours during formulation and application or during shelf life. Regard SPF15 as the minimum Sun Protection Factor that should be used. Avoid sun exposure rather than rely on a sunscreen to protect the skin. Make sure that you use a broad-spectrum sunscreen that protects against UVA and UVB rays.
What are these free radicals anyway?
A free radical is an unstable compound that can attack and injure vital cell structures. Free radicals are formed daily through normal body processes. Environmental pollutants like cigarette smoke and radiation also generate them. This leaves a molecule with an unpaired electron, which then tries to capture this needed electron from another stable molecule. Normally, the body can handle free radicals, but if antioxidants are unavailable, or if the free-radical production becomes excessive, damage can occur. Free radical damage accumulates with age, leading to wrinkling and the formation of sunspots or solar keratosis on the skin. Inside the body they make the cells more vulnerable to degenerative diseases.
Supplementing with anti-oxidants like vitamins A, C and E is advisable to help the body deal with free radicals. These vitamins give up their electrons for the good of our cells. To help fight damage and dryness on the skin these anti-oxidants should be topically applied via vitamin rich serums, whilst taking them orally will help your internal cells as well.
Changes in the skin due to age and environmental damage
We have already mentioned that UV, chemicals and pollution can lead to damage to the skin, but what exactly does this mean?
For the Epidermis
- More easily damaged as it becomes thinner, with fewer cell layers.
- Becomes dry and rough as the stratum corneum gets thicker (this is a reaction in the skin to protect against further environmental damage).
- The number of Langerhans cells decrease with age, resulting in a decreased immune response on the skin, which may account for an increase in the incidence of premalignant and malignant lesions on older skin.
- Sebaceous glands themselves do not change much with age but sebum production will decrease, leaving your skin drier.
- Diffuse hair loss due to a reduction in density of the hair follicles.
- Melanocytes are evenly distributed in young skin, however with age these melanocytes decrease in number and become more localized in certain areas, resulting in brown, blotchy macules and patches. This is commonly found in sun-exposed skin.
For the Dermis
- It becomes thinner.
- Dermal elastic fibres degenerate resulting in a loss of pliability.
- Elastosis is a result of sun-damage & ageing. As the elastosis deepens, the collagen disappears proportionally. This means that the elasticity provided by the fibrous network in the dermis is degraded and the dermis loses its pliability. Wrinkles appear first and are visible in areas of heightened muscle activity (frown lines, smoker’s line, the mouth and crow’s feet around the eyes).
- Because of the decreased thickness of the epidermis, small blood vessels in the dermis will become more obvious. Blood vessels may also increase thanks to long-standing inflammation in the superficial (papillary) dermis.
- A rise in DNA-repair protein. As we grow older, our cells accumulate DNA damage while their ability to correctly repair it declines, leading to changes in appearance associated with ageing. The cells in your body must repair up to one million DNA lesions per day from both environmental and cellular sources. Failure to properly repair DNA damage can influence not only your appearance as you age but also have other detrimental biological impacts, including the development of cancer.
- An increase in irregular pigmentation. This happens as pigmentation in dark areas is stimulated and pigment cells in pale areas are damaged by UV.
- With chronic, severe sun damage you may find that large “black heads” (comedones) occur in the oily areas of the face.
- Actinic or solar keratosis (sunspots) eventually occur due to disordered skin cell growth and, ultimately, skin cancers develop because of the impairment of the immune system.
Skin cancers
Apart from causing environmental damage to the skin, sun exposure can cause three types of cancer:
- Basal Cell Carcinoma (BCC): The most common form of skin cancer, it causes elevated, translucent, pearly bumps on the sun-exposed skin. BCC rarely metastasizes and can be removed by curettage.
- Squamous Cell Carcinoma (SCC): The second most frequent cancer type, SCC appears on the lips, face, the rim of the ears and the hands as elevated, mushroom-like or wart-like growths. It is localized and does not spread. It is removable and is sometimes treated with X-ray therapy.
- Malignant Melanoma (MM): The deadliest form of skin cancer, MM’s occurrence is doubling every year. Blue-and-green-eyed people with fair skin are at the highest risk to contract MM. Melanoma starts as flat mole-like growths. They are asymmetric, with irregular, jagged edges and have multiple colours, usually red, blue, white, brown and black.
How to support the skin?
Whilst “ageing is a privilege denied to many” as the saying goes, it doesn’t mean you have to just accept looking older than your years. There are things you can consider adding to your skincare routine:
- Vitamin A
Topical application of vitamin A for 10 days to the skin helped to increase epidermal thickness. It also prevents abnormal tissue development and the excessive development of a horny layer during epidermis metabolism. It helps the treatment of wrinkles, stimulates collagen synthesis and increases the potential for retarding ageing of skin due to ultra-violet radiation exposure. Repeated use improves texture, smoothness and firmness, maintaining a more youthful skin condition. Combine with vitamin C for the treatment of burns, acne and skin ulcers. - Vitamin C
A lack of vitamin C results in insufficient collagen and intercellular cementing substance. The vitamin also has a skin lightening effect. The topical application of vitamin C combats free-radical formation.Applying L-ascorbic acid directly to the skin also provides additional protection from UV that lasts for days. Vitamin C also prevents ultraviolet immune-suppression - a reaction that has been implicated in both melanoma and non-melanoma skin cancers. - Vitamin E
Another anti-oxidant, the tocopherol in Vitamin E helps to nourish your skin, and protects it from free radical damage. It improves the function of sebaceous glands and ameliorates excessive pigmentation in the skin. It also offers powerful protection from the sun. - Alpha Hydroxy Acids
Popularised in the 90s these may be either naturally occurring or synthetic. Examples include glycolic acid, lactic acid, malic acid and mandelic acid. Unlike beta hydroxy acids which cause continuous exfoliation and can lead to skin irritation, AHAs work through an internal cell regulating mechanism creating a stratum corneum of normal thickness. AHAs fall into the same pH as skin, which is naturally acidic at a pH of 4.2 to 5.6. This acid mantle is important in the skin being able to resist infections and chemical hazards. Whereas a more acidic solution would cause skin peeling the moderate acidity of alpha-hydroxy acids (between pH3 and 4.5) can lead to:- a reduction in the stratum corneum to normal levels
- thickening of the epidermis due to higher protein & glucose uptake in the epidermal cells leaving skin smoother and softer
- increased collagen synthesis in the dermis which means greater elasticity and an improvement in the appearance of fine lines.
- dispersal of excess pigmentation resulting in more even skin colouration.
True skin rejuvenation with Hypochlorous acid (HOCl)
HOCl is a weak acid formed by the human white blood cells and is used by the body to heal wounds and fight infection. There are several sources of HOCl in the world, however, most of these solutions are contaminated with bleach molecules due to the way the HOCl is produced. At Thoclor Labs we make our HOCl using a proprietary method that results in a stable, pure and non-toxic product containing no bleach molecules. At a pH of 5.6 this is a perfect topical solution to apply to the skin.
When our GF2 HOCl is applied to environmentally damaged skin it has the following benefits:
- The genes associated with inflammation, ageing and disease are switched off.
- Skin cells begin to function normally - collagen, elastin & melanin formation is normalised.
- Results in a smoother, more tolerant skin with fewer wrinkles, better hydration & a more even skin tone.
- Disappearance of DNA-repair protein meaning no more DNA faults when new cells are made.
- Inflammation & redness on the skin are massively reduced (great for sensitive skin or those with eczema or allergies).
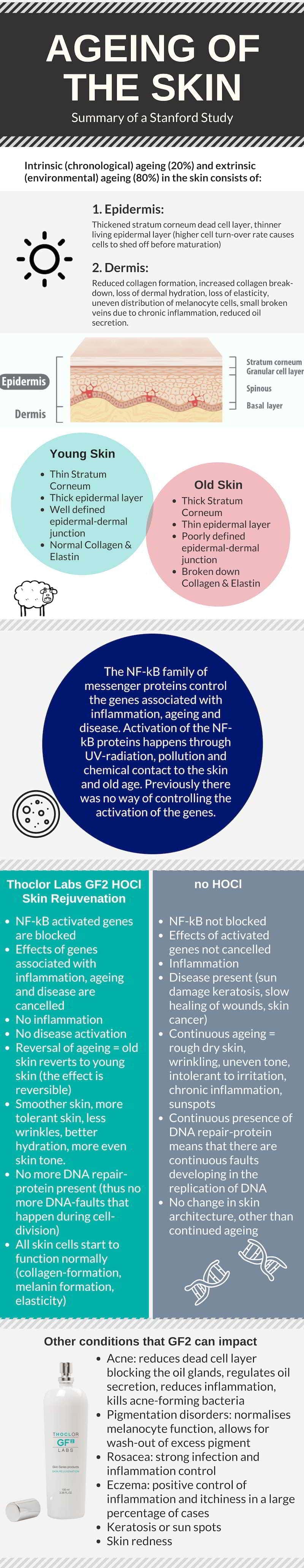
A study at Stanford University concluded that Hypochlorous acid has several transformative effects on the skin. Our GF2 stimulates a reversal of environmental damage on the skin, giving you true rejuvenation with continuous use.
Click the image below to download our infographic summarising the Stanford study findings (PDF)
References
- Role of the NF-kB Pathway in the Pathogenesis of Human Disease States. Yamamoto, Y. Current Molecular Medicine, Volume 1, Number 3, 1 July 2001, pp. 287-296(10)
- Research article: Leung H. et al. Topical hypochlorite ameliorates NF-kB mediated skin disease in mice. Department of Developmental Biology, Dept. of Dermatology and Radiation Oncology. Stanford University School of Medicine. Journal of Clinical Investigation. Vol. 123, No.12 Dec 2013.
- Fitzpatrick TB, Freedberg IM, Eisen AZ et al. Fitzpatrick’s dermatology in general medicine VII, 5th ed. New York: McGraw- Hill, 1999: 1698-703,2702-03, 2937-46
- Draelos ZK. Cosméticos em dermatologia, 2ª ed. Rio de Janeiro: Revinter, 1999: 245
- Juez JL, Gimier LP. Ciencia cosmética: bases fisiológicas y criterios prácticos, Madrid: Consejo General de Colegios Oficiales de Farmaceuticos, 1995: 212
- Draelos ZK. Cosméticos em dermatologia, Porto Alegre: Artes Médicas, 1991:158-59
- The Dermal Institute - "Structural Changes Associated with Aging Skin". http://www.dermalinstitute.com/us/library/11_article_Structural_Changes_AssociatAs_with_Aging_Skin.html
- Health Check Systems - "Understanding Free Radicals". http://www.healthchecksystems.com/antioxid.htm
- Harvard University Blog - "DNA DAMAGE AND SKIN CANCER: IT’S NOT ALL ABOUT THE SUN". November 2012. http://sitn.hms.harvard.edu/flash/2012/issue130/